Sleep is essential for our bodies to rest and repair and it’s the only time our brain gets a chance to rest, regenerate, and clean up the memories and inputs from the day. During sleep, there are distinct stages of sleep that help the brain rest and recover, and other stages allow the muscles and joints to decompress and repair daily damage.
When sleep is disrupted by not breathing well (sleep apnea, snoring, etc.) the specific stages of restful and restorative sleep are also disrupted. Over time, the brain gets overloaded with toxins, excess information that hasn’t been properly stored, etc.
 In one study from 2007[1], depression was cited to affect 20% of the adult population. At that time, the statistics also showed about 20% of adults also has Obstructive Sleep Apnea (or OSA).
In one study from 2007[1], depression was cited to affect 20% of the adult population. At that time, the statistics also showed about 20% of adults also has Obstructive Sleep Apnea (or OSA).
The prevalence of both has dramatically risen in recent years and may also reflect the inter-relationship between proper sleep and mental health. The amount of sleep disruptions, severity of being tired during the day, correlated with levels of depression.
The repeated oxygen deprivation during sleep apnea and sometimes chronic low oxygen in snorers leads to changes in brain chemistry that may lead to neurocognitive changes. Serotonin reuptake inhibitors, the mainstay of treatment for depression, may have a slight negative effect on the airway dilator muscles that are responsible for keeping the airway open while we sleep.
If someone is developing a sleep breathing disorder (due to anatomy, aging, weight gain, etc.) is it possible that SSRI’s can contribute to development or worsening of a sleep breathing disorder. New medications are always being looked at in treatment of depression.
Repeated oxygen starvation also causes significant inflammation throughout the cardiovascular system and in the brain. Inflammation chemicals called cytokines also play a role in depression.
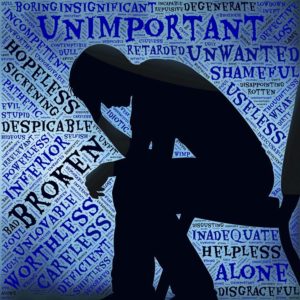 Symptoms of depression also overlap with symptoms of sleep breathing disorders including OSA (obstructive sleep apnea) such as fatigue, feeling tired, poor motivation. Patients with OSA also report difficulty concentrating, remembering information, being irritable, loss of enjoyment for life, etc.
Symptoms of depression also overlap with symptoms of sleep breathing disorders including OSA (obstructive sleep apnea) such as fatigue, feeling tired, poor motivation. Patients with OSA also report difficulty concentrating, remembering information, being irritable, loss of enjoyment for life, etc.
Snoring is one sign of a potential Sleep Breathing Disorder. Dentists trained in TMJ and Sleep Disorders can recognize the damage to the mouth, teeth, airway and TMJ and help the physician get a proper evaluation for a sleep disorder. TMJ damage from clenching and grinding of the teeth is also a well-established symptom of a sleep breathing problem. In up to 70% of patients with TMJ problems, we find a co-existent sleep disorder and vice versa. This is especially true in teenagers and younger children.
If you or someone you know has problems sleeping, with depression or anxiety that isn’t responding with medical intervention, an evaluation for TMJ and the related signs of a sleep breathing disorder would be an important step to take.
[1] Advance for Managers of respiratory Care, October 2007. Subramanian, S., MD, DABSM, FCCP




